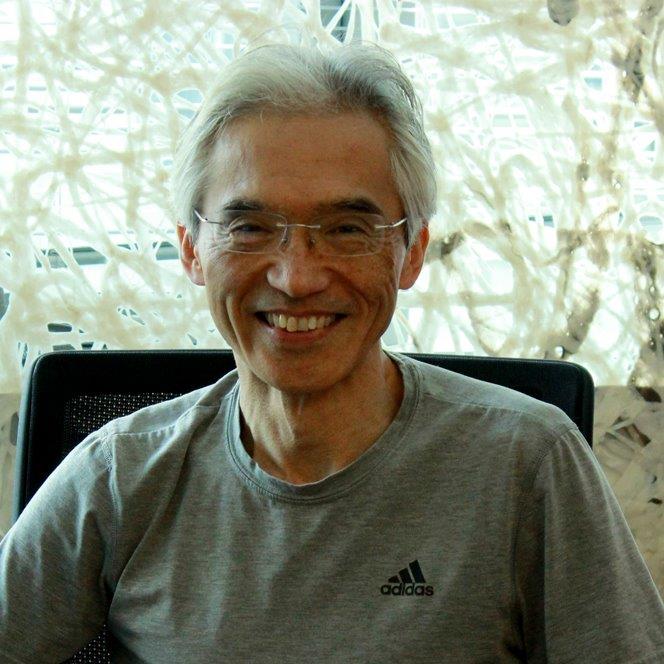
Makio Iwashima, PhD
Title/s: <p><em>Professor</em></p> <p><em>Microbiology & Immunology</em></p> <p><strong>Research Interests:</strong></p> <ul> <li>Cell biology of T cell subsets.</li> </ul>
Phone: 708-216-5816
Email: miwashima@luc.edu
Title/s: <p><em>Professor</em></p> <p><em>Microbiology & Immunology</em></p> <p><strong>Research Interests:</strong></p> <ul> <li>Cell biology of T cell subsets.</li> </ul>
Phone: 708-216-5816
Email: miwashima@luc.edu
Ph.D., Stanford University
Major Research Interests: Cell biology of T cell subsets.
In 2015, the WHO documented 4.5 million infant deaths worldwide. The infant immune system is highly tolerogenic. While infants need this immunosuppressive state to prevent inflammation and disease when they first encounter environmental microorganisms after birth, this condition also impairs the infant’s immune responses to vaccines and pathogens. Surprisingly, we still do not know how the immunosuppressive state is maintained in infants, nor the mechanisms by which children outgrow this suppression and become immune- competent adults. Moreover, many phenomena that we observe in fetus also occur in the tumor environment. To develop better care for infants, there is a critical need to understand why the infant immune system is different from the adult immune system.
We currently have three major areas of interest: 1) How does neonatal immune system adjust to the new environment after birth? 2) What is the shared property of the fetal and tumor microenvironment and how do they inhibit immune responses? 3) What does environment change the fetal and neonatal immune system?
In our recent work, we have demonstrated that human umbilical cord blood-derived cells differ in their surface antigen expression. Differing expression of these surface antigens suggests a lineage switch in these cells in cord blood versus adult blood. To understand this difference, we analyzed the expression of genes expressed by immune cells derived from cord and adult blood. Our data show expression of multiple genes differ between cord blood and adult blood cells. In this project, we will determine how such differences contribute to the characteristics of fetal/ neonatal immune system.
Transforming Growth Factor-β (TGF-β) signaling plays pivotal roles during the fetal development. Moreover, TGF-β signaling induces tumor metastasis and immune suppression. Paradoxically, TGF-β also induces inflammatory immune responses under certain conditions. Despite these significant and pleiotropic roles of TGF-β signaling in immune regulation, the molecular mechanism by which TGF-β signaling controls immune cell differentiation and suppression remain poorly understood. Our goal for this project is to elucidate how and when TGF-β is generated and find the direct targets of TGF-β signaling in activated immune cells. These studies could inform the design of therapeutics that modulate T cell responses and enhance immunity of infant and cancer patients. The outcome also will help to develop treatment of autoimmune disorders.